Over-Treatment & Overlooked Truths
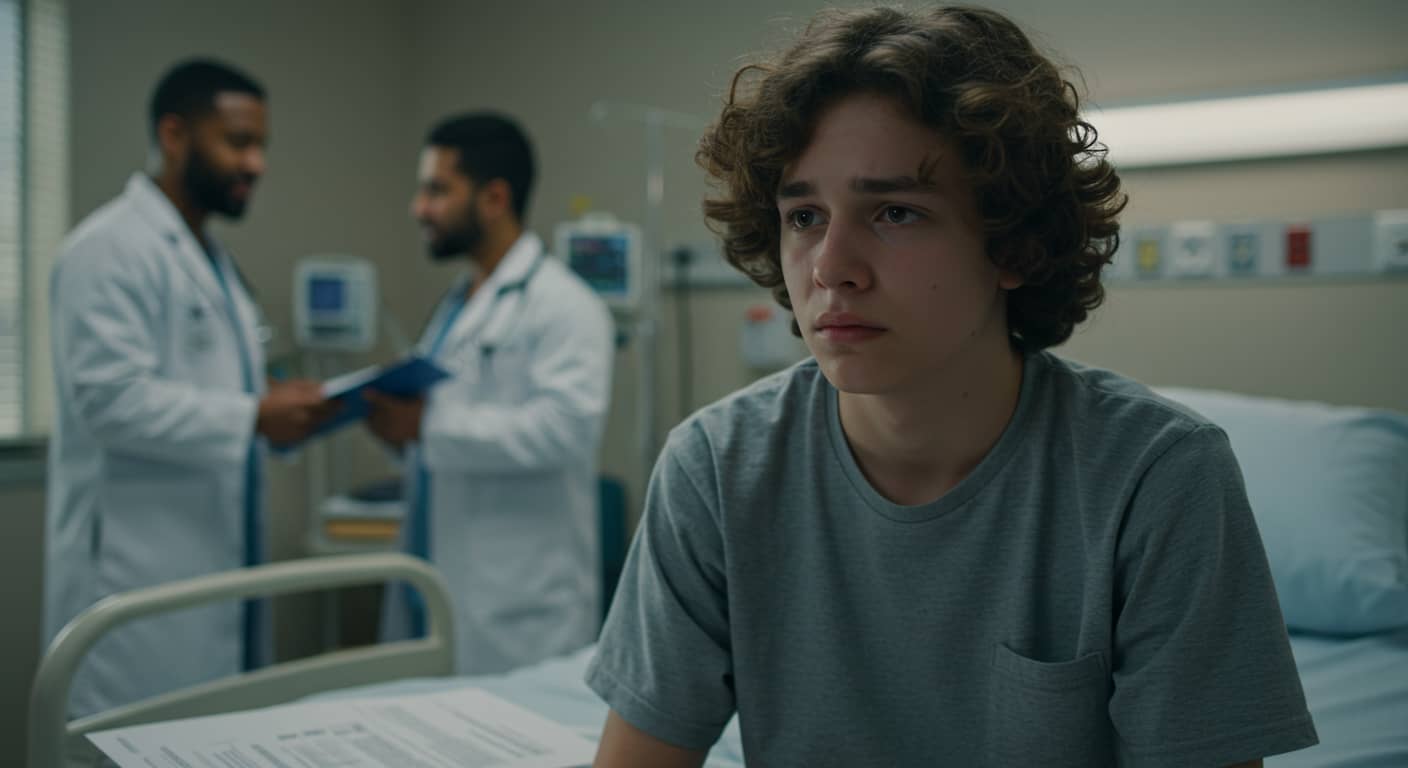
Misdiagnosed depression is alarmingly common, especially among adolescents. This isn’t always due to negligence—many physical and mental health conditions share symptoms like fatigue, sleep problems, and irritability. But when depression is mistaken for something else—or vice versa—the real issue remains untreated. This not only delays healing but may lead to unnecessary treatments that don’t help, and worse, erode a teen’s trust in medical professionals.
Mistaken Identity: Conditions That Mimic Depression
A surprising number of physical conditions mirror the signs of depression. These include anemia, diabetes, hypothyroidism, and fibromyalgia—all of which can cause fatigue, brain fog, and mood changes. Even mental disorders like ADHD, anxiety, and bipolar disorder are often confused with depression in adolescents. This overlap complicates diagnosis. A depressed teen may be treated for one thing while their real emotional distress remains hidden.
The Problem with One-Size-Fits-All Diagnoses
Of course, no parent wants to believe their child is struggling mentally, and no doctor sets out to misdiagnose a teen. But doctors are human—and often guided by their area of expertise. A pediatrician might miss emotional nuances a psychiatrist would catch. That’s why, if your gut tells you something is off, a second opinion is not only wise—it could be life-saving. Sometimes depression coexists with another condition, and both need attention.
Misdiagnosis & Racial Disparities in Teen Mental Health
Studies show that Black teens are less likely to be diagnosed with depression, often receiving care only when symptoms become extreme. This delay is rooted in systemic bias and cultural misunderstandings in medicine. Many young Black patients are misdiagnosed with behavioral issues instead of mood disorders, leading to ineffective treatment and further isolation. Mental illness doesn’t discriminate, but unfortunately, diagnosis often does.
Mental Health vs. Medical Preference
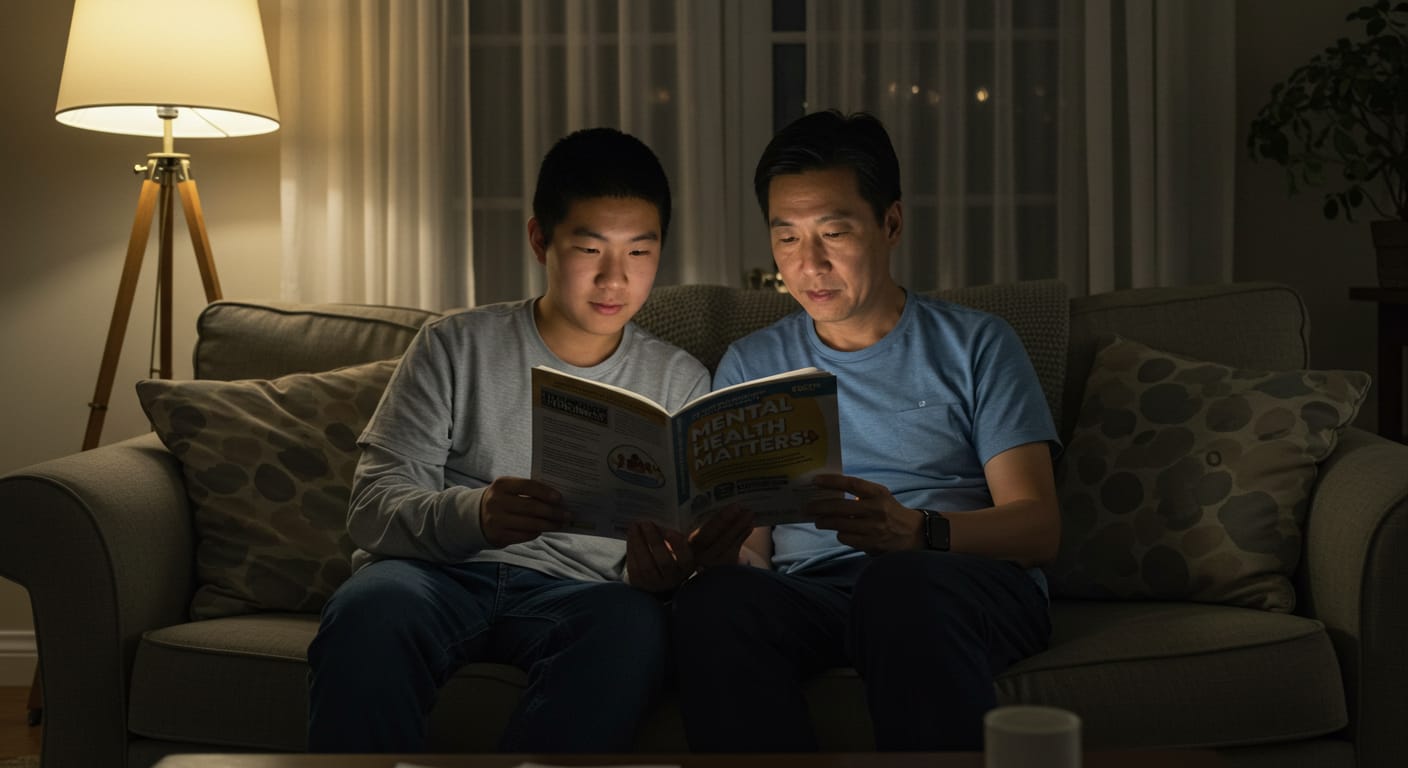
Due to stigma, families may prefer a physical diagnosis over a mental health one. Physical illness feels more tangible—more ‘real’—to many people, while depression is often misunderstood or brushed off. But this mindset is dangerous. Depression is just as legitimate and treatable as any other illness. Ignoring it doesn’t make it go away—it only allows it to grow in the dark.
When Medication Doesn’t Help: Red Flags to Watch
If your child is being treated for another condition (like anemia or hypothyroidism) but their mood stays low, or they continue showing signs like social withdrawal, hopelessness, or self-harming behavior, consider the possibility of an underlying mental health disorder. A mental health professional can spot the difference and offer more tailored support. Just because your teen seems “fine” or is high-functioning doesn’t mean they aren’t struggling.
Final Thought: Misdiagnosis Isn’t a Failure, It’s a Chance to Try Again
Don’t blame yourself—or your doctor. Misdiagnosis isn’t always malicious; it’s often a result of how complex adolescent health can be. What matters is how you respond. Validate your teen. Make your home a place where they feel safe to express confusion or sadness. Break down the stigma with words like, “It’s okay to feel this way.” And most importantly—keep asking questions. If needed, get a second opinion. You’re your child’s biggest advocate. Don’t be afraid to act like it.